A Real Claims Recovery Solution — With Zero Financial Risk
The healthcare revenue cycle was built to post money — not to verify correctness. That assumption quietly costs hospitals millions every year.
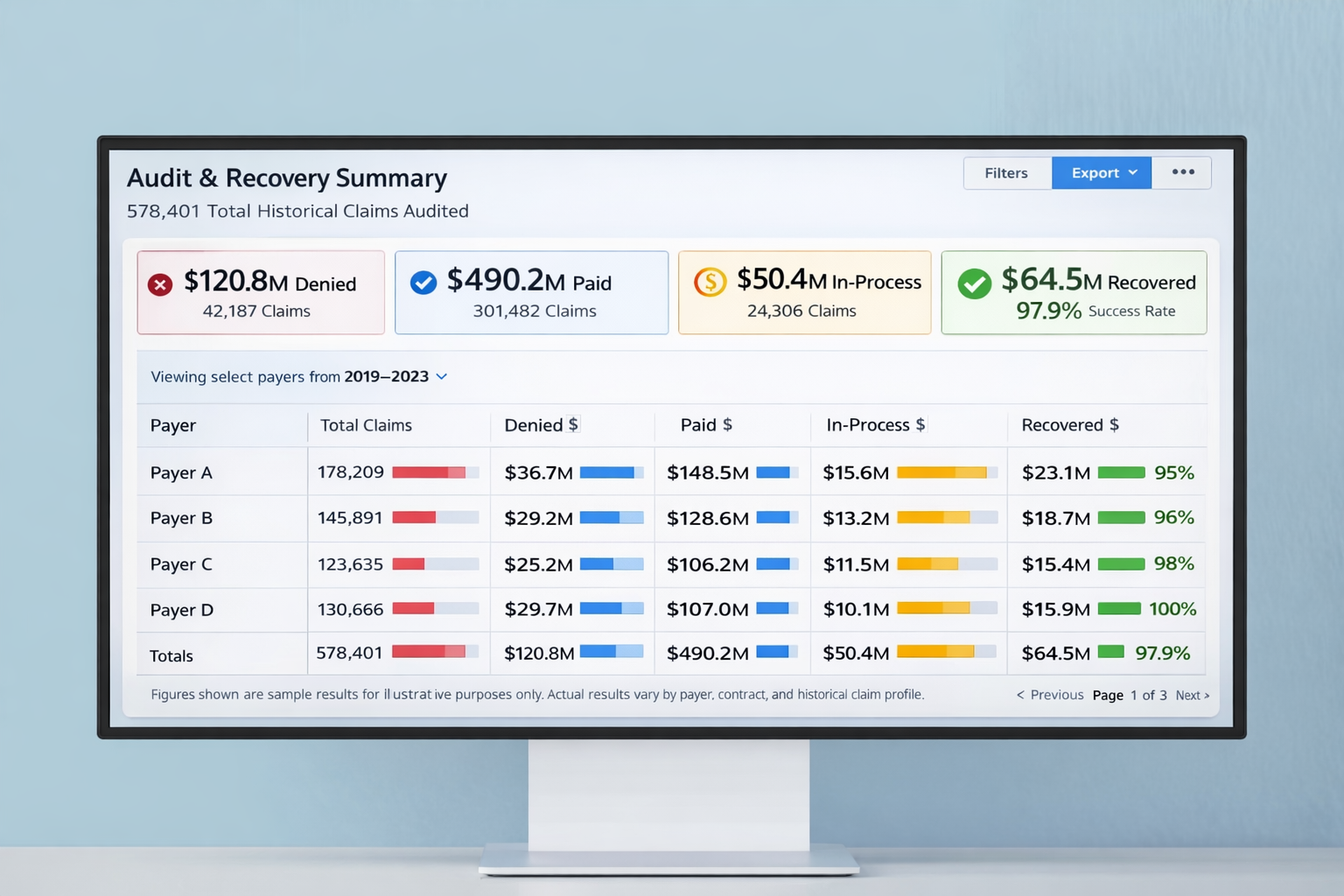
Beyond-Claims continuously audits paid and denied claims, corrects misadjudication at the service-line level, and recovers revenue previously left behind — with payment only when you actually collect.
Why this matters at the leadership level: Revenue that was previously assumed “gone” is now visible, measurable, and recoverable — changing financial conversations from conjecture to confidence.
The Platform
See everything, miss nothing: Traditional RCM reporting focuses on denials and collections totals. What’s missing is transaction correctness — whether dollars were actually paid in full.
The analytics dashboard surfaces issues hidden deep in adjudication logic so you can act on precise opportunities.
Beyond-Claims
Economics unlocked: Manual recovery efforts fail because partial payments, contract nuances, and bundled edits drain resource economics. With deterministic processing, we make every line-item actionable and economically viable.
- Audits paid and denied claims continuously
- Finds recoverable dollars at the service-line level
- Builds corrections that can be resubmitted and tracked
- Designed to make small claims economically recoverable
Beyond-Truth
From recovered dollars to real-world impact: When revenue is returned to the system, it becomes capacity — funding training, staffing, facility upgrades, and better care delivery without cutting services or raising patient costs.
Pricing
No setup fees. No minimums. No recovery — no cost. Beyond-Claims only participates when revenue is actually collected.