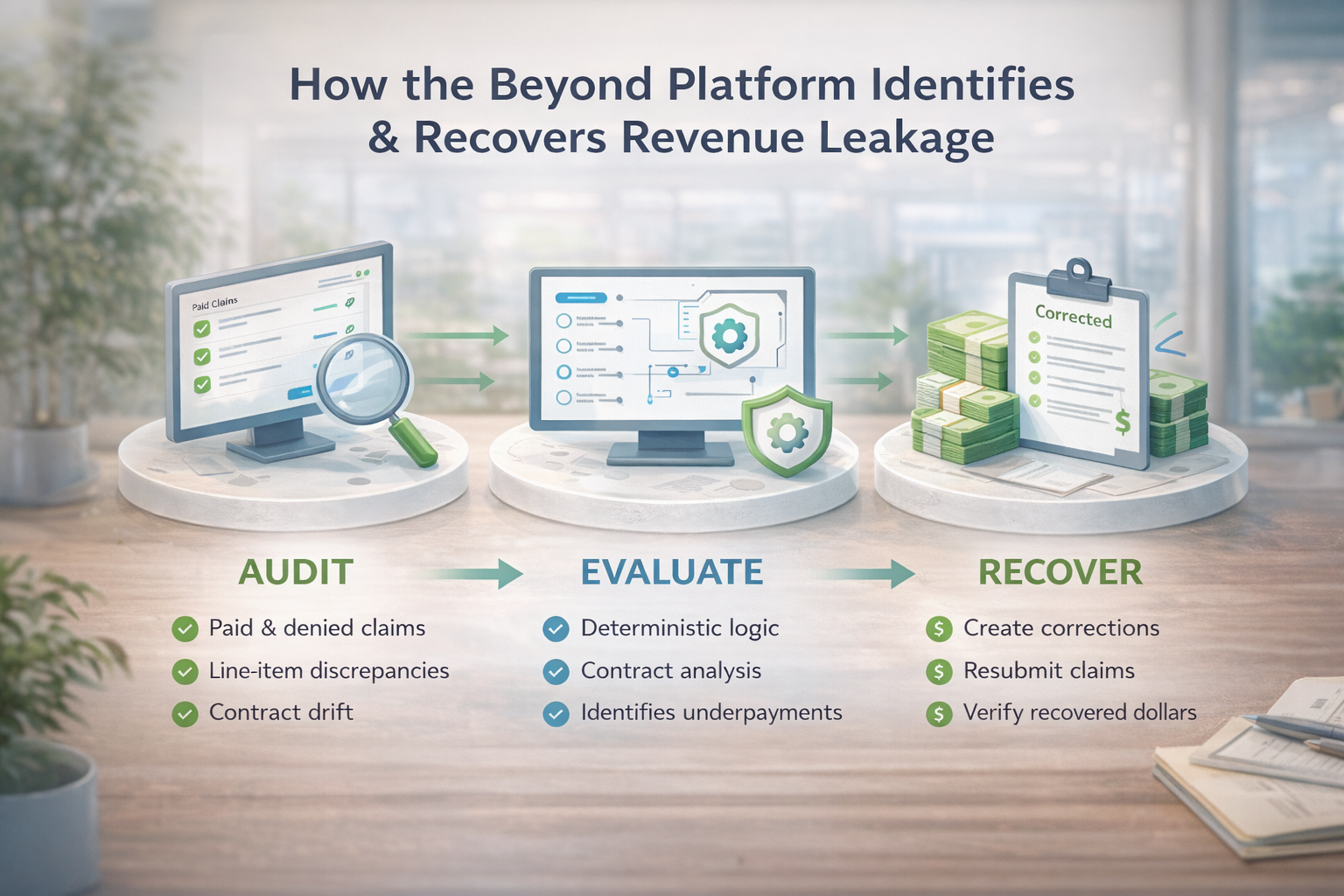
A Deterministic Platform for Revenue Integrity
The Beyond platform continuously audits paid and denied claims at the service-line level, identifies misadjudication, and enables recovery workflows that were previously invisible or uneconomical.
What the Platform Audits
The platform evaluates both denied and paid claims without relying on sampling, thresholds, or assumptions once payment posts.
- Fully denied claims
- Partially paid claims
- Paid claims with line-item discrepancies
- Claims auto-closed within tolerance thresholds
- Claims affected by contract enforcement drift
Why Errors Persist After Payment
Most revenue leakage occurs not because denials are ignored, but because paid claims are assumed to be correct.
Contract misapplication, modifier logic, bundling errors, and policy changes often affect only portions of a claim — allowing errors to survive posting and never trigger review.
How Beyond Evaluates Claims
Beyond uses deterministic, rule-based logic — not probabilistic AI — to ensure every outcome is auditable, explainable, and defensible.
- Service-line level adjudication review
- Repeatable rule enforcement
- Full traceability to source data
- No black-box scoring models
What Clients Receive
The platform delivers governed financial outcomes — not theoretical insights.
- Verified recovery opportunity by payer and service line
- Recovery tracking through payment confirmation
- Executive-ready audit transparency
- Board-appropriate financial accountability